Remember that nursery rhyme? No? That’s okay. Like many nursery rhymes, it really isn’t as baby friendly as a rhyme ought to be.
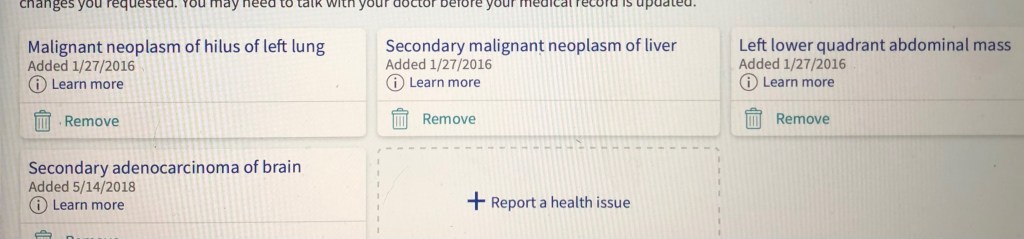
Good news! All the test results I did receive so far from my whirlwind day at Dana-Farber yesterday are just the same as May. Stable. No progression seen in chest and abdomen CT scans. And, blood tests results (except cholesterol) are very good. In the days of COVID-19 I didn’t get a same day reading of my brain MRI, but I am expecting that to be okay too. (Power of positive thinking, and I’ve no new symptoms.)
Because of a mix-up in scheduling, DF wasn’t able to get my testing all done in a timeframe that made it possible for my superhero chauffeur to drive to Boston from home, wait in the car, and drive back home in one day. That presented a big problem in my mind as the only buildings other than ours that I’ve been in since March 8 are 2 health facilities. So, ugh. Decisions, decisions. Postpone? Twelve weeks is already the longest allowed time between appointments when in this clinical trial, and from our perspective it is plenty long enough. So no postponing. Because I learned about Thursday’s appointment Monday afternoon (it was first scheduled for next week, which I thought seemed odd because that was 13 weeks), it was really too late to ask someone to go with us. And besides, you know… COVID-19. (Not fair to ask of someone.) Ugh, okay. Well, in May everyone we saw on the streets wore a mask, and at DF I felt as safe as one could in these times. The Inn at Longwood, a hotel a block from DF, is accustomed to medical patients staying there, so they must be careful. Fingers crossed. I packed enough food and water for two days, and decided we could get to a room with no/minimal contact and sanitize surfaces when we got there. (I did not take our own bedding.)
We left home at 2:45 AM. We always allow some time for traffic. For the second time, traffic, even going into the city, was light. (I think many may be still not working, not traveling, working from home.) We already knew that Dan wouldn’t be allowed in with me. (Typically during the day of appointments, there’s down time to be together, I know he’s just outside the room waiting, and he’ll be at the appointment when we hear the results. But, that can’t be in the days of COVID-19.) His plan was to sit in the car until he/we could go to the hotel. Fun, huh? Me? Even more fun, if possible. The day (and trip) worked out pretty well. But to me it seemed like lots of exposure to lots of spaces and people. All masked. All distancing. Here’s a recount:
8:00 AM start from parking garage.
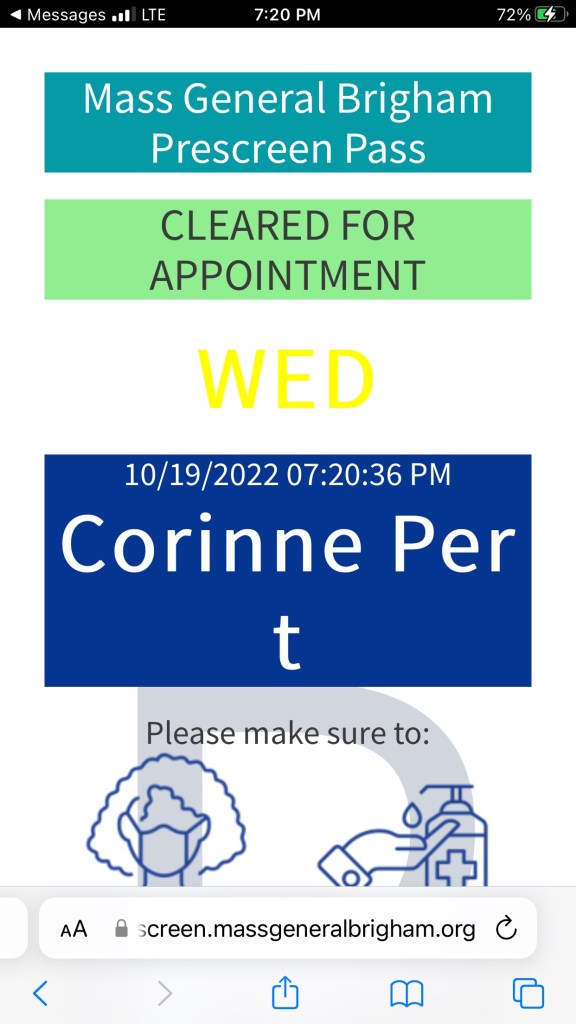
Elevator (alone) to Floor 1 Yawkey. COVID-19 screening questions, get surgical mask (everyone, even if yours is comparable). (Two different people) Get badge showing I cleared screening, learn that because we’re a little early I must wait in cafeteria before going to lab.
Elevator to Yawkey Floor 3. Sit in cafeteria, touching only my phone to text Dan and call hotel.
Elevator to Yawkey Floor 2. Check in with receptionist for labs. Get the usual clip on badge that can find me, answer same COVID-19 questions. Sit in waiting area. Go to lab, nurse draws blood and puts in IV.
Elevator to P2, walk through “tunnel” to Dana. Screeners there see my badge.
Elevator to Dana L1. Check in for CT scan. Same COVID-19 questions. Sit in waiting area. (Everywhere chairs are spaced, and the number of people is much lower than typical. Makes me wonder how many people are putting off treatment. You can’t zoom scans.)
Called into room where typical CT scan questions are asked and to get nasty drink. (Person again got drink, and wasn’t wearing gloves. Yes I want a straw, sanitary I hope inside that paper.)
Back to waiting room. Same chair is empty. Wipe hand sanitizer on bottle. Spend 30 minutes drinking nasty drink.
9:50 AM CT scan. IV unwrapped and flushed, scans. Dye in IV, scans. IV flushed and wrapped. (I still wonder how you can taste the saline so quickly or at all when flushing the IV. I need to google and watch an animated video of that.) CT tech says MRI called and I can go there now instead of 1:00. Okay! Wait, we’re going to try to check in at hotel. Send quick text to Dan.
Use bathroom on Dana L1 before leaving.
Elevator to Dana 3. Check in with MRI receptionist. Same COVID-19 questions. Sit in waiting area.
Tech comes out to get me. Changing room and locker. All off but undies – hospital johnny, pants, and socks.
Into prep room (my term) where MRI questions are asked and IV unwrapped and flushed. Same Tech.
Into to MRI room. Mask upside down. (The nosepiece will show, but on my chinny chin chin.) Lie down, two techs (I’m not sure what their professional title is.) tuck me in. Nighty, nighty. Halfway through I’m hauled out (don’t move!) for dye to be put in IV. When done, back to changing room. Take clothes from locker, dress. Go back through waiting area.
Walk across bridge (indoor) from Dana to Yawkey.
Elevator to P5. Hand sanitize and get in car, interrupting Dan’s lunch.
11:30 AM Hotel parking garage, check in, sanitize room cards, elevator to Floor 7, enter room, and wipe down as much as sensible (maybe more). The room looked very, very clean when we entered. Things like remote were wrapped in plastic (changed each time).
Put food in fridge, have lunch and rest in hotel room. Both unexpected and appreciated. Usually there’s no time for me to eat (or I can’t before a test/procedure) and I never really rest on DF day.
2:30 Elevator to lobby. Walk one block to DF. Everyone is masked and distances.
DF Floor 1. Ask if I need screening again or new mask. Young man handing out masks says no. Good thing I have on a new, clean surgical mask.
Elevator to Floor 10. (one other person). Check in at receptionist for EKG and Dr. appointment. Same COVID-19 questions. Sit in waiting area. Very few people in a very large space. Feels so different. Thinking about going to my appointment without Dan, I am grateful that the people coming to their first appointment are allowed to have a companion. And no, I’m not going to FaceTime the appointment. If there’s hard news, I want to be with Dan when he learns about it. Okay, enough of that. Good news is what we got.
Into to room with nurse for vitals to be taken. No I don’t want the kg to lb conversion, thanks.
Into different room for EKG. Lie on bed/table Socks down, shirt up. Sticky pads here, there, and almost everywhere. Two nurses (I’m quite sure they are nurses) – one supervising the other who does the EKG.
Back to waiting room. Different chair.
Another person takes me to the exam room for my appointment. This day I saw a NP. When I first started at DF I frequently saw Margaret, so I was excited to see her, and always am happy to see Nurse Dawn (clinical trial nurse). Margaret and Dawn come in together. We talk about tests (all good, MRI reading next day) high cholesterol (it is a known med side effect, but as Margaret said, “We don’t want for your heart to be damaged by the medication”, maybe trying yet another new med for the cholesterol.) We discuss other side effects (neuropathy is “okay”, weight gain makes many aspects of life difficult). Up on exam table/bed. Lungs and heart sound good. Off to get next 12 weeks of trial drug.
Elevator to Floor 2, one other person. Push button at trial drug window of pharmacy. Not ready. Sit in waiting room. Sit in waiting room. Sit in waiting room. 45 minutes. Get med. No touch, expect bag to drop in my bag. (Can’t walk the streets with a clear bag of pills, even if they won’t do anything good for nearly 100% of the population.)
Elevator to Floor 1 (Never see stairs offered as choice.), one other person. Out the door! Yay!
Walk back to hotel. More people, still masked and distancing. Remarkable and impressive. (Especially since at the Rusty Lantern in Augusta where we filled the gas tank, no one going in and out of the convenience store had a mask.)
Into to lobby and up the elevator to Floor 7. Into room, wash hands, change clothes. Brew tea.
Nothing to it, right? A full day. I am not complaining, just hoping to help people understand. It’s tough and tricky. It’s tougher and trickier in the days of COVID-19. And I really have it very easy compared to many. I am grateful I am a very healthy 63 year old, living well with stage IV lung cancer. I am grateful little ROS1 is treatable, knocked on his fanny for now by the honorable Lady Lorlatinib. I can deal with the side effects, as they are currently. I am grateful for my Dana Farber team. A special thing I learned – Dr. Ghandi, my first DF oncologist has returned to DF! Not Floor 10, but back, so that is very good news for DF. We will forever be grateful to her for giving us so much hope at a time when others are made to feel so empty of any hope.
And, now here we are. Back at camp, finding joy in the everyday every day. At 5:00 AM we left the parking garage in Boston, stopped once to fill up the gas tank (Dan, hand sanitizer used), and were greeted by happy goats and dachshunds! And, a little more sanitizing because our spoiled puppies had overnight guests. Thanks Mandy and LL, for staying over. (They DO NOT like being left, even when checked on. Peace of mind for all of us.)
Thanks for reading, and for your support. Be kind to others, please. Try to find joy in your day every day, it helps. And please vote. If by mail, vote early! Love to all.