LONG POST- NOT URGENT. Information sharing!
Since January 3, 2016 I’ve had a few procedures and many tests (scans, MRIs mostly). I thought it might be helpful to describe these from the perspective of a person who doesn’t really get too worked up about things like this. Me.
You can read the description of any procedure and test online, and I think that’s a pretty good idea. I mean, how is one to know if you have any questions if you really can’t picture what’s planned? I imagine we’ve all had the experience when the technician or doctor asks if you have any questions, and you’re still stuck on the first thing they said about what was about to happen. But, if you prefer just going with it, no need to check it out first online. And, when you’re desperate for the information the procedure or test might provide, you may truly want to just go with it. In either case, if you do go online to check out how the procedure is done, don’t get stuck on the risks. You’re going to have this done, the doctors (and you by consent) have determined that the benefits way outweigh the risks. And seriously, in my case, it’s been a “no brainer”. I know some of what I’ve had done can cause cancer, but I’ll take living long enough to participate in a study on that when it does catch up with me.
So I’ll try to do this chronologically, beginning with the lifesaving x-ray. The one that showed my tumor was done at a walk-in clinic on a winter Sunday afternoon. It’s an “electromagnetic wave of high energy and very short wavelength, which is able to pass through many materials opaque to light” that’s used to take photos of what you can’t see. You lie on the table, the tech leaves the room (to protect themselves) and click, click – that’s it! Quick, easy, painless, and oh so informative. Why, it can find broken bones and lung tumors!
Got a “cough, cough” for months? Ask for an x-ray just to be sure it’s not a tumor. Low dose CT scans are available too, especially if you are “at risk” for lung cancer.
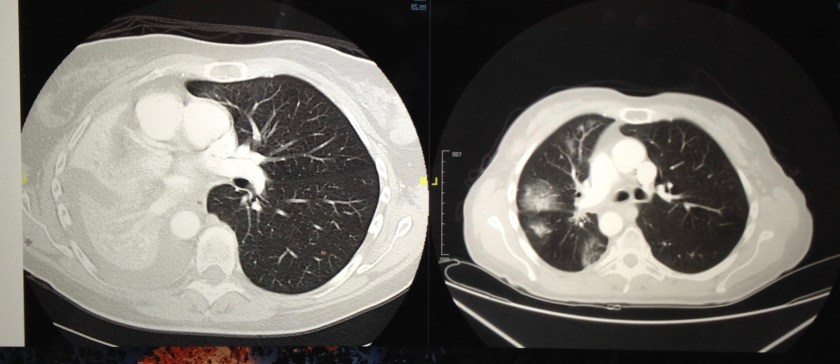
CT scan (sometimes called CAT scan) “A computerized tomography (CT) scan combines a series of X-ray images taken from different angles and uses computer processing to create cross-sectional images, or slices, of the bones, blood vessels and soft tissues inside your body. CT scan images provide more detailed information than plain X-rays do.” (Mayo Clinic) Well, I guess it’s just a fancy x-ray that gives more detailed information. Mine are all “with contrast” – an intravenous and/or an oral “dye” is used to enhance the scan/x-ray. My first one in this journey was at my local hospital.
I’ve had many CT scans of my chest and abdomen at a few different clinics/hospitals. At Dana-Farber they trust you to come clothed in “NO metal” clothing. Sometimes they ask about underwire bras, zippers, or pocket contents, just to be sure and safe. Here’s how my CT scan appointments have gone. Nothing to eat, and only clear liquids for two hours before. If you are having oral contrast and haven’t gotten it ahead of time, you arrive an hour early, check in and get your tasty drink. (It’s not so bad, sometimes seems like a lot.) At some point a nurse/tech will take you to put in an intravenous catheter (unless you have a port) in your arm/hand. It is a small, flexible tube put into the vein so the contrast can be Putin or blood can be drawn out. The vein inside my right elbow is great, so mine go there, get taped on, wrapped, and are used for the CT and any other tests, blood draws, etc. that day. Nearly painless, just a little jab. Next! At some places I’ve had to undress, leaving just my underwear, socks, and shoes on, and put on a johnny (short gown fastened in the back) for the scan. Then you go into the scan room (which is probably cold) and lie on a table/bed with a big machine shaped like a donut around it. It’s very open. You lie still and move to the donut, hold your breath for about three seconds, and move out. A couple pictures and then the technician comes back in to start the IV contrast, He/ she returns to safety, two more pics, and then they flush out the IV or take it out if you don’t need it again that day, and you’re on way. Drink lots of water that day to flush the contrast out of your system!
This explanation from radiology info.org is great for understanding CT scan, MRI, and PET scan process. “The CT scanner is typically a large, box-like machine with a hole, or short tunnel, in the center. You will lie on a narrow examination table that slides into and out of this tunnel. Rotating around you, the x-ray tube and electronic x-ray detectors are located opposite each other in a ring, called a gantry. The computer workstation that processes the imaging information is located in a separate control room, where the technologist operates the scanner and monitors your examination in direct visual contact and usually with the ability to hear and talk to you with the use of a speaker and microphone.”
Bronchoscopy That first CT confirmed that I had a tumor, so I went to a pulmonologist (lung specialist) who decided to do a bronchoscopy: “an endoscopic technique of visualizing the inside of the airways for diagnostic and therapeutic purposes. An instrument (bronchoscope) is inserted into the airways, usually through the nose or mouth.” This was a relatively easy (for me) day surgery procedure. I was given something for anesthesia – “In the practice of medicine anesthesia or anaesthesia is a state of temporary induced loss of sensation or awareness.” ( I don’t remember this, I guess it worked!)
A tube, with an instrument in a smaller tube inside the larger tube, was put in my mouth and into my lung. The doctor used the instrument to look around and to snip some tumor tissue for pathology. I think this process took less than an hour. I woke up in recovery, was told I may have a sore throat and to call if any coughing up blood, and home I went. After sleeping off the anesthesia, I was fine (from that anyway), no sore throat even.
The pathology report took many, many days (from this facility anyway), and the sample ended up being sent on to Brigham and Women’s because it was “inconclusive, rare, abnormal” and need further examination. (What?!? Now you begin to understand why we took ourselves to Boston.)
After seeing the tumor, the pulmonologist decided it was a good idea to have a Brain MRI and PET scan (To see if I “lit up” anywhere else. Places where there are cellular changes “light up” in the image.)
Brain MRI (Magnetic Resonance Imaging) “Magnetic resonance imaging (MRI) of the head uses a powerful magnetic field, radio waves and a computer to produce detailed pictures of the brain and other cranial structures that are clearer and more detailed than other imaging methods. This exam does not use ionizing radiation and may require an injection of a contrast material called gadolinium, which is less likely to cause an allergic reaction than iodinated contrast material.” (compared to CT scan with contrast) radiology info.org
I’ve had about 10 of these now, so here’s a description from an earlier post, with additional thoughts. “This means taking off everything but my undies, putting on a johnny, having an IV put in . Then into the cold room, and getting up on the table in the right spot, cushions beside my ears, a “hockey mask” clamped over my face, and into the tube I slide. Oh yes, you can choose music or earplugs to slightly deafen the sound. I choose earplugs now. (Music on that first one.) And, you are given a bulb to squeeze if you need anything (because of course the techs are safe away in another room watching you). The techs talk some to let you know how much longer, etc. Probably if you’re not still, they tell you. Halfway through I’m slid out to put the contrast dye in my IV. After listening to some pretty strange and very repetitive noises for 40 minutes, I get out of the tube, have the IV removed, dress, and go.” Some people have difficulty with the idea and feeling of having the open mask over their face, the closeness of the “tube”, and the noise. Luckily for me, I don’t. I can only say that the techs are just a squeeze away, however snug it is when you go in won’t get any snugger, focusing on breathing slowly is calming. I count the repetitions of the different sounds to pass the time!
PET scan (Positron Emission Tomography) “Positron emission tomography (PET) uses small amounts of radioactive materials called radiotracers, a special camera and a computer to help evaluate your organ and tissue functions. By identifying body changes at the cellular level, PET may detect the early onset of disease before it is evident on other imaging tests.”radiology info.org I’ve only had one of these.
For a PET scan you can have nothing to eat and only clear liquids for a few hours before. You can wear no jewelry, and they’ll ask about metal in your body (true for all scans, MRIs). You CAN leave your wedding ring on! You are asked to remove all clothing except undies and put on a johnny. This procedure requires an IV for the radiotracer. The radiotracer is injected and you need to just sit and relax for about an hour, I guess while it travels through your body. Then you go into the room for the scan, and as I remember, it is like a CT scan (above) from there, except it looks at your whole body (not your brain) instead of a specific area.
Because the PET scan showed enhancement in my liver, one of the first things that happened after I went to Dana Farber was a liver biopsy to make sure that it was lung cancer metastasized to my liver and not another cancer or something else.
Liver Biopsy This procedure was much easier than I thought it would be. It is done as outpatient/day surgery. I had mine at Brighams. No food or drink after midnight, undressed/wear johnny, IV put in. For this I was sedated, but fully aware. ( If I had been too nervous, talkative, agitated- I’m sure with the push of a button, I’d have been asleep.)
The liver biopsy is a needle biopsy. The procedure is ultrasound guided. “Ultrasound imaging uses sound waves to produce pictures of the inside of the body. After you are positioned on the examination table, the radiologist (a physician specifically trained to supervise and interpret radiology examinations) or sonographer will apply a warm water-based gel to the area of the body being studied. The gel will help the transducer make secure contact with the body and eliminate air pockets between the transducer and the skin that can block the sound waves from passing into your body. The transducer is placed on the body and moved back and forth over the area of interest until the desired images are captured.” radiology info.org
So, while you are lying on your back, the doctor doing the procedure is standing very close to your right side, and does the above process to your abdomen to get a clear look at your liver. Then he/she cleans the area (just below the right rib cage) and gives you a shot or two of novocaine to numb the area. Next he makes a small incision for the needle. You hold your breath (no, really) while he inserts a long needle and gets what he needs, and pulls the needle out. You then go to the recovery room where you have to lie still on your right side (due to bleeding possibility) for several hours. Then, when we were done I was tired, a little sore where the incision was, and couldn’t lift over 10 pounds for a week. Really much easier than anticipated and quite painless.
Okay, in trying to think about what else I’ve had for procedures, I think the only other besides radiation treatment, which you can read about at length in an earlier post, is a lumbar puncture (aka spinal tap) which I needed after the cancer crept into the meninges. This was done to see if the beast had spread into my entire central nervous system by looking for cancer cells in the spinal fluid. (The fluid that’s drawn is lab analyzed.) It is a test that isn’t too effective (reliability, 41% sensitivity), but I guess it is a simple way to look for cancer when there’s that concern and no related symptoms.
Lumbar puncture I had mine done at Dana Farber. No special prep, just changed into a gown (I like the idea of wearing a gown better than johnny.) Here’s a good description of the procedure from mayoclinc.org . “You lie on your side with your knees drawn up to your chest, or you sit and lean forward on a stable surface. These positions flex your back, widening the spaces between your vertebrae and making it easier for your doctor to insert the needle.Your back is washed with antiseptic soap or iodine and covered with a sterile sheet.
During the procedure
- A local anesthetic is injected into your lower back to numb the puncture site before the needle is inserted. The local anesthetic will sting briefly as it’s injected.
- A thin, hollow needle is inserted between the two lower vertebrae (lumbar region), through the spinal membrane (dura) and into the spinal canal. You may feel pressure in your back during this part of the procedure.
- Once the needle is in place, you may be asked to change your position slightly.
- The cerebrospinal fluid pressure is measured, a small amount of fluid is withdrawn, and the pressure is measured again. If needed, a drug or substance is injected.
- The needle is removed, and the puncture site is covered with a bandage.”
I was sitting, leaning forward. The doctor did spend quite a bit of time at the start tapping my spine with her hand and marking me with a marker. She wanted to find just the right spot to slide the needle to withdraw the fluid. While the needle was in I did feel quite a bit of pressure, but not pain. When all done I laid still for 20 mins and then was pretty quiet for the rest of that day and evening. I had no lingering effects from this. And, when lab results were back – no cancer cells were found in my spinal fluid. (Since then I’ve been put on the targeted therapy drug Lorlatinib and SHE has reduced the cancer in my meninges by 75%!
I know I’ve said this before, but it is true – I’m lucky. An acquired cell mutation caused my cancer to take off and spread, but it is because of this that I can take a targeted therapy drug – a pill(s) once or twice per day. The drug acts as a guided missile, attacking only those mutated cells, not all cells like chemotherapy does. So, I know that I’ve not had some of the tests, procedures, and treatments that many lung cancer patients have to endure. I hope that this field is changing so rapidly that soon we all will be able to treat lung cancer as a chronic disease, not a terminal one, until a cure is found. At just under two years since diagnosis, I’m am blessed to feel well enough to enjoy life with family and friends. Feeling joyful and filled with gratitude daily.